*For kids it’s anything but normal.
By Patrick Gaulier, LMSW & Leah Diebel, LLMSW
Last year, Michigan parents and students were faced with a very difficult adjustment from in-person education to attending school virtually. As many schools push for more time in the classroom, parents and students are again making an adjustment, this time back to in-person learning. After a year of virtual classes where students didn’t have to leave their bedroom or home, walking into a school with hundreds of other children or teens can feel like a daunting task. As a parent, dropping your (nervous) child off after months of having them home is equally daunting. Even kids and parents that normally don’t experience social anxiety (or anxiety period) may feel nervous because they are out of practice. It’s normal to feel that way and there are ways to help the return to school go more smoothly for parents and children.
Prepare for school to be different from what they remember.
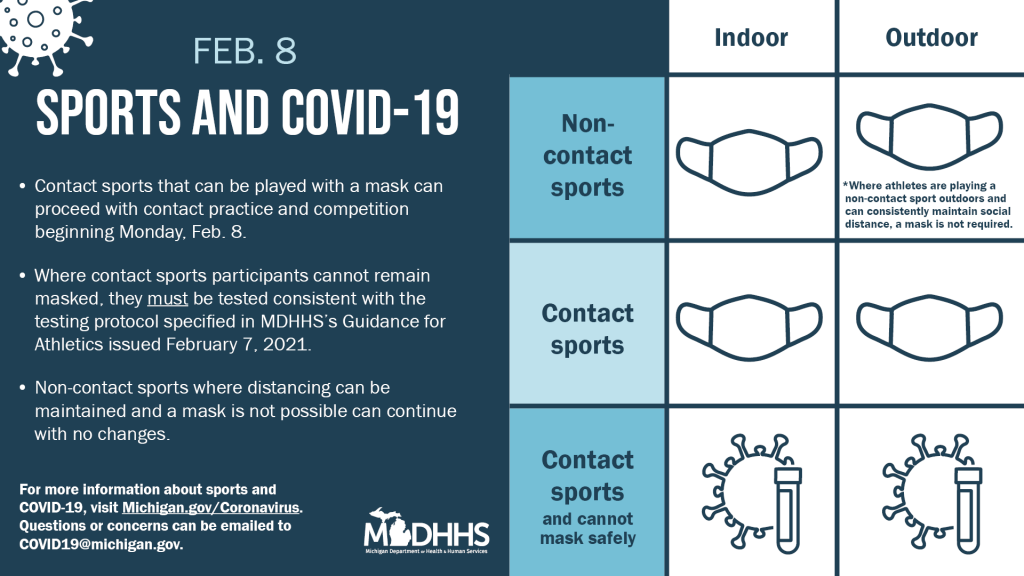
The school children left last spring is not the same place they will be returning to. Everyone will be wearing masks, friends will have distance between them, there may even be plexiglass shields, and lunchtime and recess will be a very different experience. Uncertainty around what school will look like upon their return will be a source of anxiety for children and teens, so the more information they have (at their level) the better. Talk to your kids about the new rules in place and how they feel about them. Try to get answers to their questions prior to their first day back in the classroom.
Let them worry.
Collectively, we say we are returning to “normal”, but really, we’re not. Kids are returning to school, but it won’t be what they remember as normal. The most normal thing about this whole process is worrying. Everyone has worries and parents can help children to see worrying is a normal part of life. Parents can help children manage worry and anxiety by asking open-ended questions like “what happened at school today?” or “what did you do at recess today?” or “did you see anything interesting on social media today?” Children may not be ready to share their feelings or answers to their questions, but they know you are ready to listen when they are. The most important takeaway is to not minimize or discount your children’s anxiety.
Create opportunities for conversations.
As you prepare as a family for the return to in-person learning, be sure to give your children an opportunity to voice their concerns and excitement as well. Plan to sit down for device-free dinners where conversations can happen. Spend a few extra minutes tucking them in at night and ask them how they are feeling about upcoming changes. For teens a chat while driving is an opportunity to talk without forced eye contact. Schedule an outing with children either individually or as a family, depending on how your child best communicates, where they have dedicated time where they can feel heard.
Brush up on social skills.
For some kids, it’s been a while since they had face to face interactions with other students, teachers and staff at their school. For younger kids, try role playing some basic greetings and conversations they can have with someone they haven’t seen is a while. Talk about some different conversations starters and questions they can ask. They should also think about a couple things they would want to share with friends. Going into school prepared can help kids manage the anxiety that comes with the change from virtual interactions to facet-to-face.
Create a new routine and stick to it.
Since so much about the school day will be different, the daily routine should evolve, not disappear. Structure and routine will provide stability in times of uncertainty. Kids should wake up early enough to complete their morning routine and parents should model structure by also waking up and preparing for the day. It won’t be acceptable to walk around in pajamas at school, so it shouldn’t happen at home as children get ready to make the change from home learning to classroom learning. If children are returning to virtual classes, they can still go through their morning routine even if their commute is to a desk at home.
Know when they/you need more help.
If you think your child is struggling or may need more help than you are able to provide, the IHA Pediatric Behavioral Health Care team is here for you and your children. They will work in collaboration with your child’s IHA pediatrician to improve your child or adolescent’s overall health as well as helping the family understand the child’s development. IHA Pediatric Behavioral Health Specialists are available for video appointments through any IHA Pediatric practice.