Get your questions answered here.
The COVID-19 vaccines are our best shot for ending the pandemic. But as expected with anything new, you may have some questions before you schedule your vaccine. We’ve compiled the most frequently asked questions we’re hearing about the COVID-19 vaccines in our vaccine clinics. Get the facts and then get your shot!
How do I get a COVID-19 vaccine?
Patients over the age of 18 can schedule their COVID-19 vaccine online here:
Patients age 16 to 17 can only schedule at specific clinic locations, please ensure the clinic says *16-17 before proceeding to schedule online. If you schedule at a clinic that does not have the capability to vaccinate a 16 or 17-year-old, your vaccine appointment will be canceled and there is no guarantee we will be able to accommodate you at a different location.
Can I choose which COVID-19 vaccine I get?
No, IHA & St. Joe’s Medical Group have received a supply of each of the currently approved COVID-19 vaccines, however the daily supply at each vaccine clinic changes, so we are not able to determine ahead of time which will be available and which you will receive. Our staff will help you schedule your second dose of the vaccine when you receive your first.
Will I be charged when I receive the COVID-19 vaccine at IHA?
No. The COVID-19 vaccine is free of charge to all people living in the United States, regardless of their immigration or health insurance status.
Can I get the COVID-19 vaccine if I have an underlying condition?
Vaccination is an important consideration for adults of any age with certain underlying medical conditions because they are at increased risk for severe illness from COVID-19. People with underlying medical conditions can receive a COVID-19 vaccine as long as they have not had an immediate or severe allergic reaction to a COVID-19 vaccine or to any of the ingredients in the vaccine.
What happens if I have an allergic reaction to the COVID-19 vaccine?
After you receive your COVID-19 vaccine, you will sit in a waiting area for monitoring with IHA providers present, for 15 minutes. If at any point you aren’t feeling well, communicate with an IHA provider and they will get you the care you need immediately. If you experience a severe allergic reaction after leaving a vaccine site, call 9-1-1 or go to the nearest Emergency Room.
Should I get the vaccine if I had COVID-19?
Yes. You should get the COVID-19 vaccine whether or not you’ve previously tested positive for COVID-19. The vaccine will produce a stronger immune system response than a natural infection.
I am currently sick with COVID-19, can I get vaccinated?
No. People with COVID-19 who have symptoms should wait to be vaccinated until they have recovered from their illness and have met the criteria for discontinuing isolation; those without symptoms should also wait until they meet the criteria before getting vaccinated. This guidance also applies to people who get COVID-19 before getting their second dose of vaccine.
Who should NOT get the COVID-19 vaccine?
You should not receive the COVID-19 vaccine if you had an allergic reaction after a previous dose of the vaccine or had a severe allergic reaction to any ingredient of the vaccine.
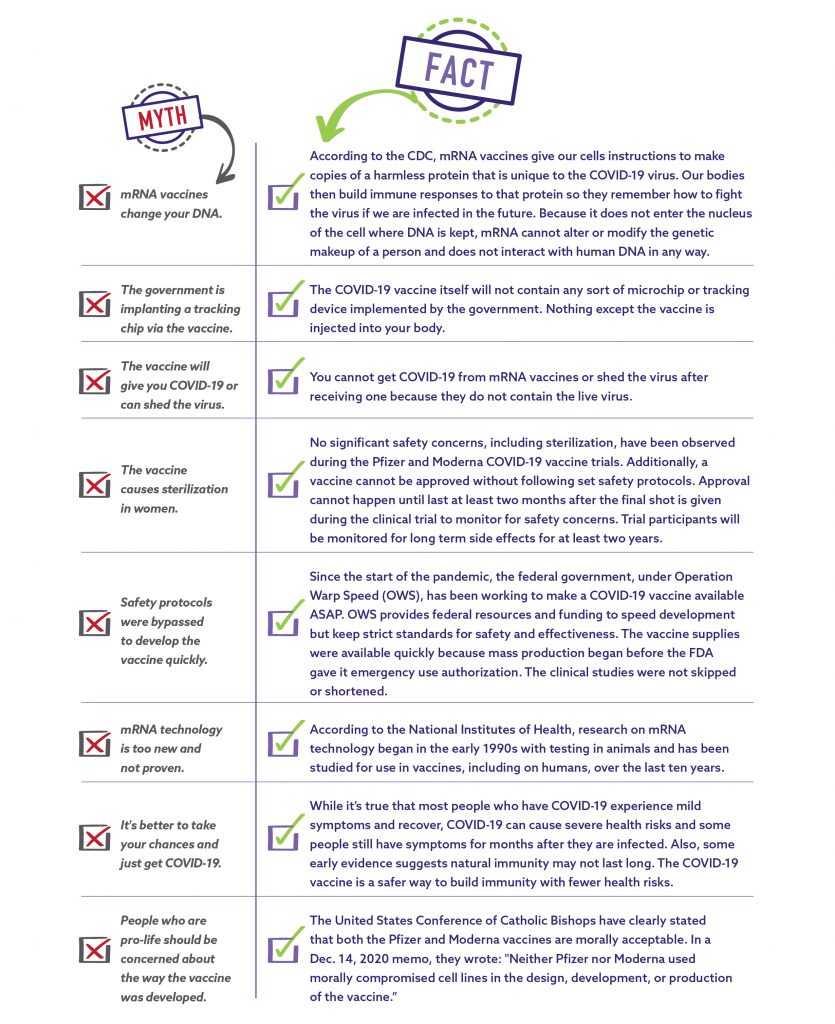
What are the ingredients in the COVID-19 vaccines?
The Pfizer-BioNTech COVID-19 Vaccine includes the following ingredients: mRNA, lipids ((4- hydroxybutyl)azanediyl)bis(hexane-6,1-diyl)bis(2-hexyldecanoate), 2 [(polyethylene glycol)-2000]-N,N-ditetradecylacetamide, 1,2-Distearoyl-sn-glycero-3-phosphocholine, and cholesterol), potassium chloride, monobasic potassium phosphate, sodium chloride, dibasic sodium phosphate dihydrate, and sucrose.
The Moderna COVID-19 Vaccine contains the following ingredients: messenger ribonucleic acid (mRNA), lipids (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC]), tromethamine, tromethamine hydrochloride, acetic acid, sodium acetate trihydrate, and sucrose.